Abstract
BACKGROUND: There is a pressing need for standardized frailty assessments in patients with newly diagnosed acute myeloid leukemia (AML), especially to observe whether disease characteristics and outcomes differ from patients treated in clinical trials. However, frailty assessments are rarely done in busy oncology clinics, calling for more innovative tools to evaluate health status in clinical databases. The Veterans Affairs Frailty Index (VA-FI) is a validated electronic measure of frailty derived entirely from administrative claims and electronic health records data that has previously been associated with survival in veterans with lung cancer and multiple myeloma. The aim of this study was to use the VA-FI to measure the prevalence of frailty in veterans with AML in the national VA Healthcare System, determining whether frail patients have inferior survival compared to non-frail veterans.
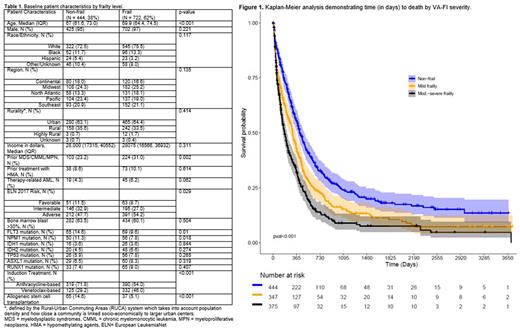
METHODS: This was a retrospective cohort study of veterans with newly diagnosed AML who were newly treated between January 1, 2012 and April 1, 2022. Patients with acute promyelocytic leukemia (APL) or those who did not receive their initial therapy within the VA were excluded. Induction regimens included anthracycline-based or venetoclax-based combinations. The VA-FI measures frailty via diagnostic and procedure codes that represent 31 aging-related health deficits spanning morbidity, function, cognition, sensory, and other, with scores computed as the proportion of potential health deficits that are present in each veteran. Using validated cut-points, patients were categorized as non-frail (VA-FI ≤ 0.2) or frail (VA-FI > 0.2), with frail patients further categorized as mildly frail (VA-FI > 0.2 and ≤ 0.3) or moderate-severely frail (VA-FI > 0.3) in our survival analysis. We evaluated the association between frailty and overall survival after initiation of treatment using Kaplan-Meier analysis and Cox proportional hazards regression models, first unadjusted and then adjusted for all covariates.
RESULTS: Our study included 1,166 veterans; 722 (62%) were classified as frail and 444 (38%) as non-frail by the VA-FI (Table 1). Compared to non-frail patients, frail patients tended to be older, have a prior myeloid disorder, present with adverse risk AML, and have higher rates of intensive care unit admissions (3.42 admissions per 5 frail person-years, 95% confidence interval [CI] = 3.1-3.76 compared to 2.72 admissions per 5 non-frail person-years, 95% CI = 2.42-3.06). Non-frail patients were more likely to have received anthracycline-based induction (versus venetoclax-based induction) compared to frail patients. Median follow-up in the study population was 252.5 days and 898 (77%) veterans died. Moderate-severely frail veterans (median survival = 179 days, 95% CI = 149-217) had significantly worse survival than mildly frail (median survival 306 days, 95% CI = 262-354) and non-frail veterans (median survival = 417 days, 95% CI = 380-485, log-rank p-value < 0.001; Figure 1). In univariable Cox regression, mildly frail veterans had a 1.38 times higher hazard of death (95% CI = 1.18-1.63, p<0.001) compared to non-frail veterans; and moderately-severe frail veterans had 1.85 times higher hazard (95% CI = 1.57-2.16, p<0.001). This association was maintained after adjusting for age, gender, race/ethnicity, region, rurality, European LeukemiaNet (ELN) 2017 risk classification, bone marrow blast percent, secondary or therapy-related AML, prior treatment with a hypomethylating agent, type of induction therapy, and transplantation status (mild frailty hazard ratio [HR] = 1.24, 95% CI = 1.05-1.46, p=0.011; moderate-severe frailty HR = 1.55, 95% CI = 1.31-1.83, p<0.001).
CONCLUSION: Measured using the VA-FI, frailty was prevalent among veterans with newly diagnosed and treated AML and associated with several baseline markers of disease risk. The VA-FI strongly predicted survival, independently of age, sociodemographic variables, markers of disease risk, type of induction therapy, and transplantation status. Our findings support using the VA-FI to retrospectively assess outcomes in frail veterans treated with AML therapies proven in clinical trial populations, and the VA-FI may help oncologists to better measure frailty in clinical practice for informing prognosis and treatment decisions. Future studies will focus on the impact of frailty on treatment outcomes.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal